Mini-incision and plication cure hydrocele technique: A less invasive surgical variation
Anthony-Joe Nassour1,2,3, Darius Ashrafi1,3, Dinesl Patel1,2,3.
1Department of Urology , Bankstown-Lidcombe Hospital, Sydney, Australia; 2Department of Urology, Canterbury Hospital, Sydney, Australia; 3University of New South Wales, Sydney, Australia
Introduction: Idiopathic hydroceles are the commonest cause of chronic benign scrotal swelling, affecting 1% of adult men. The popular Jaboulay technique (1902) is curative and remains the standard for most surgeons. However, it is associated with significant morbidity and has a reported recurrence rate of 5%. Various minimally invasive approaches have been described with fewer reported complications but limited efficacy, with unacceptable recurrence rates requiring multiple treatments. We describe a novel mini-incision and plication (MIP) cure hydrocele technique and report on our morbidity and recurrence.
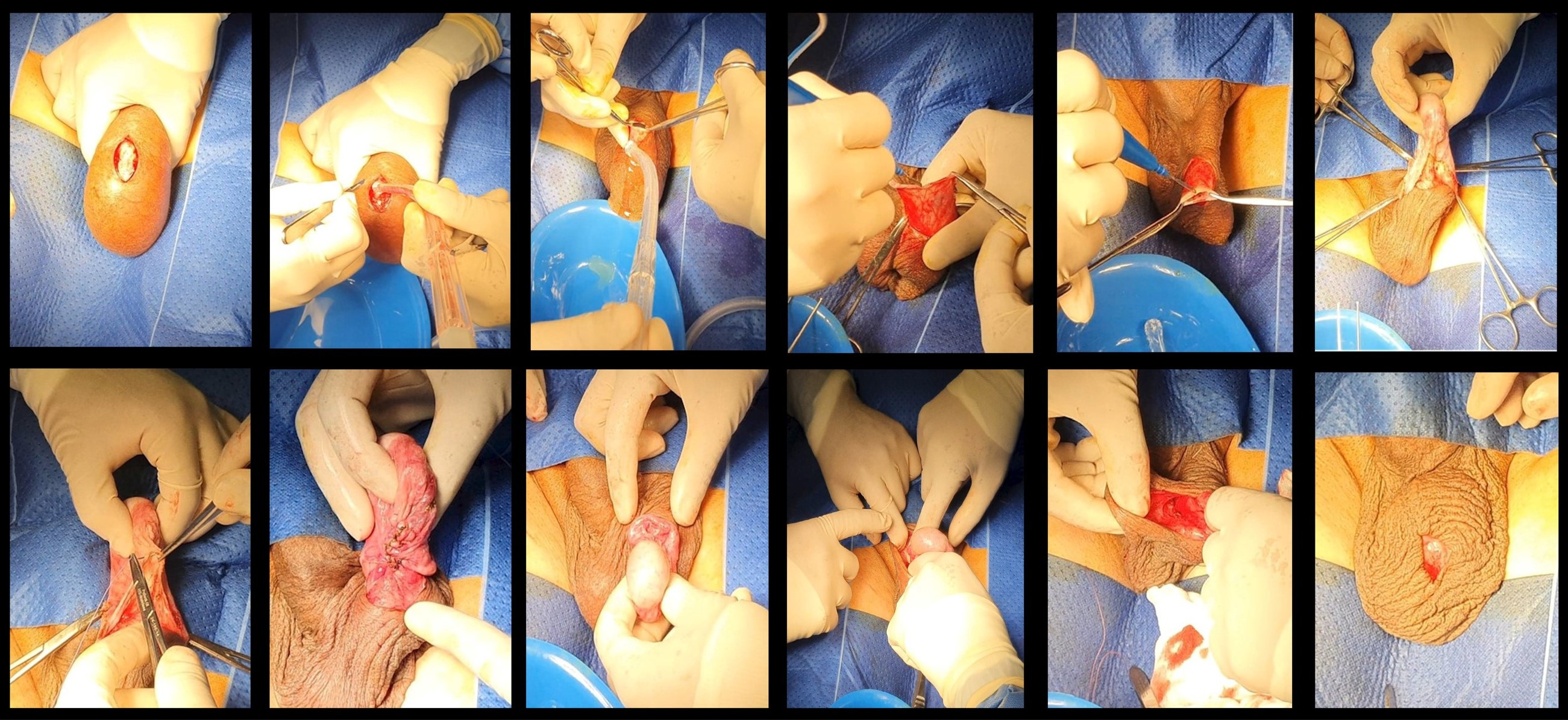
Methods: A retrospective, single-surgeon audit was conducted on patients that underwent the MIP at two hospitals in Sydney between January 2013 and December 2020. This technique is performed using a standard minor-ops tray. Key operative steps include: small midline incision, early drainage of hydrocele, complete incision of the anterior hydrocele wall, delivery of testis, eversion and posterior plication of the bisected hydrocele sac, repositioning of testis, and standard closure. Routine postoperative followup takes place at one and three months. Recurrence was defined to be any visible or palpable fluid collection that appeared and persisted within three months after surgery.
Results: A total of 92 men underwent MIP for symptomatic hydrocele; 83% had idiopathic hydroceles. Hydrocele size ranged from 50–1200 cc (57% were grouped as large and very large). Most (93%) were day-only procedures; 7% remained overnight due to spinal anesthesia. Zero drains were left and 22% had transient post-surgical edema that resolved by three months. Hematoma that did not require a return to the operating room developed in 4.3%. Only 1% developed a recurrence, resulting in a redo procedure at three years.
Conclusions: The MIP approach achieves eversion and plication with minimal hydrocele manipulation, a small incision, and no drains compared to Jaboulay. It provides excellent results independent of hydrocele size, with a lower complication rate and a recurrence rate of 1%.